Goldilocks and Prostate Cancer
Why a patient’s column?
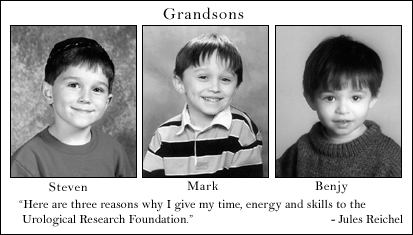
This is not a doctor’s column. I am a patient of Dr. Catalona and a member of the URF Board. This column attempts to provide a patient’s perspective on prostate cancer to the readers of Quest.
To review my prior columns please see Dr. Catalona’s Website, www.drcatalona.com. Insert my name in the “Quest Articles” search engine.
Being treated “just right”: Small tumor volume, Lowest PSA cutoff region
 When Goldilocks entered the house of the three bears, she uttered the world famous phrases: “This porridge is too hot.” “This porridge is too cold.” “This porridge is just right.” Even a child understands that some things are too much, some are too little, and some are just right.
When Goldilocks entered the house of the three bears, she uttered the world famous phrases: “This porridge is too hot.” “This porridge is too cold.” “This porridge is just right.” Even a child understands that some things are too much, some are too little, and some are just right.
We, too, are looking for “just right” treatment of prostate cancer. Our doctors are getting closer to finding such an approach. Although no study has as yet described a complete answer, some early results may be helpful to patients.
The potential change in approach to screening and treatment results primarily from two newer understandings:
1) Diagnosing and treating prostate cancer when tumor volume is small plays a large part in controlling possible recurrence after treatment (by surgery, for example); and
2) screening and treatment in the lowest “PSA cutoff” region of 2.6 to 4.0ng/ml offers the potential of much lower rates of recurrence.
Being treated “too hot” or “too cold”
Being treated “too hot” results from waiting too long. The prostate cancer is no longer localized and the rates of recurrence greatly increase. The available systemic treatments that are then required have more uncertain outcomes and usually are much more harsh.
Being treated “too cold” occurs when no treatment may have been needed. The problem for our doctors and us is that small changes in clinical stage, tumor volume, and Gleason score, can shift us from being too cold to too hot.
Because no one can reliably assess the risk of a too cold cancer becoming too hot, decisions about how to treat these more mild cancers are very difficult.
How good is “just right” treatment?
My suggestion is that being treated “just right” may mean that we have at least 95% probability of non-recurrence in 10 years, or at least 90% in more difficult cases.
These goals are about 10-30% better than current best practice. The studies I cite are for possible recurrence after surgical treatment.
Some potentially “just right” results
My last article in QUEST referred to a study that considered tumor volume. The information used a December 2002 report from Dr. Patrick Walsh’s and his data from 1149 patients.
Smaller tumor volumes greatly improved the chance for 10-year non-recurrence, and in Senator John Kerry’s case of a stage T1c (non-palpable tumor) cancer, Walsh predicted a 98% probability of 10-year non-recurrence after surgery primarily because of the small tumor volume and lower Gleason Score (less than 7).
In general, Walsh reported 96% rates of non-recurrence at both 5 and 10 years for the less severe (smaller tumor, lower Gleason score) fraction of T1c patients. That’s encouraging but it’s not clear how to screen for such men.
Dr. Catalona reports the rates of recurrence for over 3000 of his patients based on their tumor volume. This data is for all patients, not just the group identified in Walsh’s study. He found that with the smallest tumor volumes, i.e. less than 10% of the prostate, 94% of the men were non-recurrent after 5 years and 88% were non-recurrent after 10 years.
Eighty-eight per cent rate of non-recurrence for the whole population might be close to a “just right” answer. However, in Catalona 1999, he reported on 1778 of these patients and found that with treatment in the lowest PSA screening region from 2.6 to 4.0ng/ml, the non-recurrence rate was 90% (not 94%, as above with the smallest tumors) after 5 years. This lower non-recurrence rate corresponds to a tumor volume of 10-20% of the prostate, instead of less than 10%.
Therefore, even if this lowest PSA cutoff region is used for screening, many men will not have the smallest size tumors and will have higher rates of recurrence than “just right”.
Opportunities in the lowest PSA cutoff region
If doctors are to treat patients while we have small tumors, then they must determine when such small tumors exist.
Many suggested approaches to finding men while their tumors are small are being developed, but the only established method at this time is to begin screening in the lowest PSA cutoff region of 2.6 to 4.0ng/ml, since normally PSA readings are directly correlated to tumor volume.
Screening men in the lowest PSA cutoff region has the potential for finding cancer when it is highly treatable as reported in Catalona June 2000. In this study, 98% of men who had detected cancer (by biopsy) either had organ-confined disease (81% of the cases), or tumors that might be considered “potentially insignificant” (17% of the cases). Such a high rate of nominally treatable cancer offers a promising opportunity for excellent long-term results.
Avoiding the need for so many biopsies to find insignificant cancer remains a technical issue. The tumor volume in this lowest PSA cutoff region was about 40% smaller than for tumors in the PSA region from 4.0 to 10ng/ml (the more common region for concern), which is consistent with the desire to treat while the tumors are small.
Unfortunately, we’ve seen above that the tumors are not as small as the smallest (less than 10% of prostate volume) tumors that had the best outcomes, and even in this lowest region for screening, 14% of the patients had Gleason Scores of 7 or higher, and such scores corresponds to higher rates of recurrence, even with organ-confined disease.
An attempt to find these more aggressive tumors in this lowest PSA screening region, for stage T1c men, was reported in another recent study. All of the men were tested using the free-total PSA test.
If their percent-free PSA was less than 27%, they were biopsied. About half of the men had positive biopsies, and all positive biopsies were for clinically significant tumors.
The use of free-total PSA testing may find a large fraction of the more aggressive cancers, and combining it with the opportunity to have small tumor volumes in this lowest PSA screening region, may be helpful.
Where do the doctors now stand in establishing “just right” treatment?
We can now understand why it is believed that very high rates of long-term non-recurrence after surgery are possible, and that the detection of important cancers can be found when their tumor volumes are smaller by using the lowest PSA cutoff region for screening and treatment.
However, screening in the lowest PSA region still leaves open serious problems. We would have hoped that working in the lowest screening region was sufficient to find all significant tumors since it corresponds to a region of smaller tumor volumes.
However, we have seen that the tumor volume is not as small in this region as one would hope, and also that a significant number of more aggressive tumors will be found. How then can we find “just right” treatment?
One suggested approach to overcoming these problems is to begin screening in the lowest PSA cutoff region, but at an earlier age. Some doctors have suggested age 40.
We would hope that there is some early time at which even very aggressive tumors are small enough to be totally eliminated by treatment. However, treatment of men as young as 40 will require great care, since any lasting side effects will be viewed as even more debilitating by such young men.
It is a unique time in the medical treatment of prostate cancer.
It is the first time when at least a few doctors, including Dr. Catalona, have modern databases of 10-year patient outcomes.
It is the first time when these alternative treatment approaches can be studied using existing data.
It should therefore not be too long before doctors can describe the screening and treatment rules that allow all future patients to achieve very high rates of long-term non-recurrence what Ive been calling “just right” treatment.
Putting this information together as a new standard of care will be a great day for future patients. We will feel as relieved as our friend Goldilocks felt when she escaped from her bears.
Feedback
You are encouraged to offer comments or ask questions about this column by contacting Dr. Catalona at his Website: www.drcatalona.com, sending me an e-mail at jules105@aol.com. Please include the word “QUEST” in the subject line when sending me an e-mail.
Click here to read the next article, Revolution in Screening for Prostate Cancer, in the One Man to Another series from Jules Reichel.











